The Lancet: Prof. You Li and Wang Xin’s team, together with international collaborators, revealed the global disease burden of and risk factors for acute lower respiratory infections (ALRI) caused by respiratory syncytial virus (RSV) in preterm infants and young children in 2019
On February 14th, 2024, Prof. You Li and Xin Wang research group from School of Public Health, Nanjing Medical University and Prof. Harish Nair from University of Edinburgh published an article titled "Global disease burden of and risk factors for acute lower respiratory infections caused by respiratory syncytial virus in preterm infants and young children in 2019: a systematic review and meta-analysis of aggregated and individual participant data" on The Lancet. The findings provided important evidence for the optimisation of strategies for prevention and clinical management of RSV-associated ALRI in preterm infants and young children.
Children born prematurely (i.e., with a gestational age of less than 37 weeks), which account for more than one in every ten livebirths globally (ranging from 9–13% across regions), are particularly vulnerable to RSV-associated ALRI and severe disease because they have a less mature immune system, smaller airways, diminished maternal antibody transfer, and higher risk of bronchopulmonary dysplasia than term children. There have been major advances in the development of novel RSV prophylactic products targeting infants; long-acting monoclonal antibody (Nirsevimab) and maternal vaccine products (RSVpreF) were licensed in the USA and Europe in the recent two years. Passive immunisation of infants under 6 months of age with nirsevimab and vaccination of pregnant women with RSVpreF could be a cost-effective strategy for protecting infants during their first RSV season. Understanding the global disease burden of (and the risk factors for) RSV-associated ALRI in preterm infants and young children is essential for the design of an optimal RSV prophylaxis strategy.
Given current regional reports on RSV associated ALRI hospitalization burden focusing primarily on Europe and other high-income countries; and global systematic reviews collecting individual participant-level data were scare. This study aimed to RSV associated ALRI hospitalization burden and risk factors through collecting 47 studies from the literature and 17 studies with individual participant-level data from the international collaborators. The researchers estimated RSV-associated ALRI incidence in community, hospital admission, in-hospital mortality, and overall mortality among children under 2 years born prematurely, and identify risk factors in perinatal, sociodemographic, household factors, and underlying medical conditions for RSV-associated ALRI incidence, hospital admission, and three severity outcome groups (longer hospital stay [>4 days], use of supplemental oxygen and mechanical ventilation, or intensive care unit admission).
The study found that among early preterm infants, the RSV-associated ALRI incidence rate and hospitalization rate were significantly higher (rate ratio [RR] ranging from 1.69 to 3.87 across different age groups and outcomes) than for all infants born at any gestational age. In the second year of life, early preterm infants and young children had a similar incidence rate but still a significantly higher hospitalization rate (RR 2·26 [95% UR 1·27–3·98]) compared with all infants and young children. Late preterm infants had higher RSV hospitalization rate in the first 6 months (RR 1.93 [1.11–3.26]). Preterm infants face a disproportionately high burden of RSV-associated disease, accounting for 25% of RSV hospitalization burden.
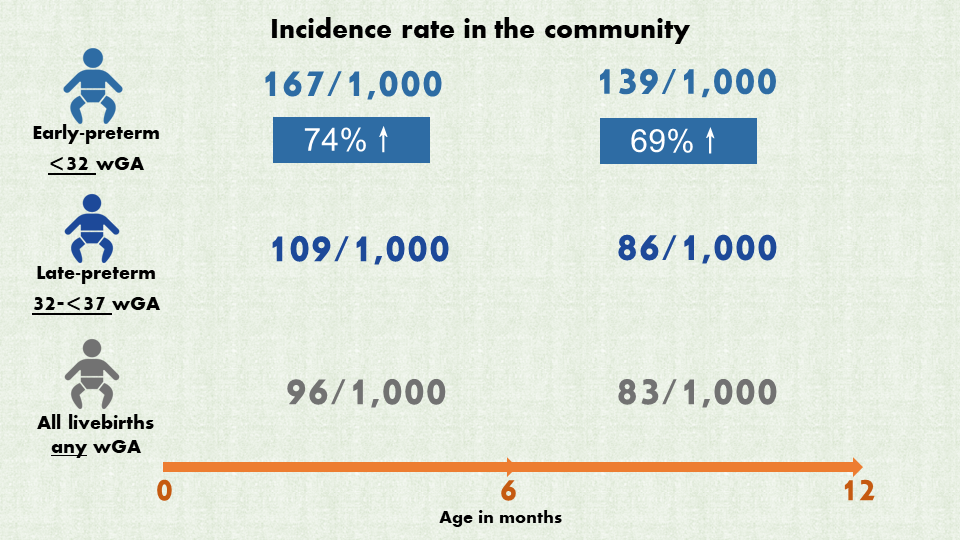

Figure 1. Global burden of infections in community and hospitalizations due to RSV-associated ALRI in preterm infants and all infants younger than 2 years
The factors identified to be associated with RSV-associated ALRI incidence were mainly perinatal and sociodemographic characteristics, and factors associated with severe outcomes from infection were mainly underlying medical conditions including congenital heart disease, tracheostomy, bronchopulmonary dysplasia, chronic lung disease, or Down syndrome (with ORs ranging from 1.40 to 4.23).

Figure 2. Risk factors for RSV-associated ALRI community episodes and hospital admissions
Compared with huge gap in the ratio of RSV-associated ALRI incidence to hospitalization rates between developing and industrialised countries observed in general children under 5 years (Li et al. Lancet 2022). In this study, a broadly similar RSV incidence and hospitalization rates was observed; this suggests that preterm infants might have better access to the inpatient health-care services than the general infants in LMICs, and possibly higher priority for admission compared with term infants.
Furthermore, the similar in-hospital case fatality ratio (CFR) between developing and industrialised countries observed in this study might be a result of survivor bias (rather than indicating similar quality of health-care provision), i.e., preterm infants who died with particular comorbidities during the neonatal period in developing countries might have survived if they had been in industrialised countries with better access to and quality of health care.
The Lancet Journal invited David Torres-Fernandez and Prof. Quique Bassat from Universitat de Barcelona commented this paper, they said “Wang and colleagues’ study provides valuable data in the highly vulnerable but neglected preterm infant population, highlighting the enormous geographical inequities in health-care assistance”.
Prof. Xin Wang and You Li from School of Public Health, Nanjing medical university are the co-first authors of the paper. Prof. Harish Nair from Centre for Global Health, Usher Institute, University of Edinburgh is the corresponding author. The research was supported by EU Innovative Medicines Initiative Respiratory Syncytial Virus Consortium in Europe (RESCEU).
Original link:https://authors.elsevier.com/sd/article/S0140-6736(24)00138-7
Comment:https://www.sciencedirect.com/science/article/abs/pii/S014067362400254X

